Introduction
In the UK, screening programmes are crucial for early
detection of breast and cervical cancer. Muslim women’s
attendance to these programmes falls below the national
average (1), increasing the risk of delayed diagnosis, and
thus exacerbating health inequalities. This study
explores the barriers that Muslim women face in
accessing screening programmes, in order to develop
initiatives to increase engagement within this population
and consequently tackle morbidity and mortality.
Methods
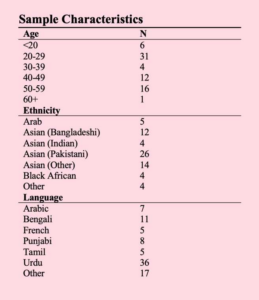
A preliminary online survey was conducted for Muslim
women to explore their understanding of women’s
cancers. Following this, an in-person breast cancer
awareness workshop, Think Pink, was completed at a
mosque in London. This was advertised in local
mosques, through community groups, and on social
media. Bilingual presenters conducted the workshop,
with resources provided in numerous languages. verbal
feedback was compiled before and after the workshop to
ascertain the understanding of attendees.
Results
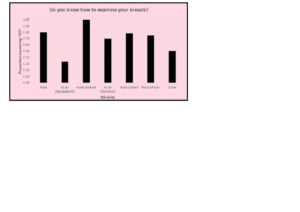
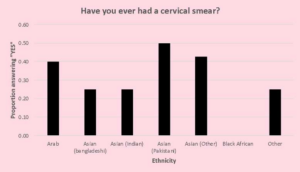
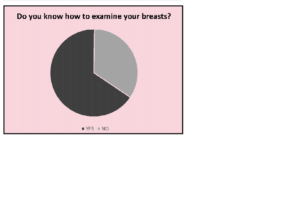
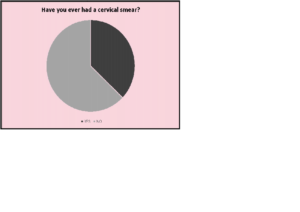
69 Muslim women aged 25-70, of varying ethnicities,
completed the survey. One-third of participants did not
know how to examine their breasts and two-thirds had
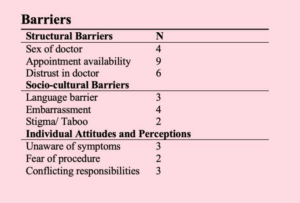
not undergone a cervical smear. The notable barriers to
accessing care included: the negative attitudes of doctors;
interaction with male doctors; family responsibilities; waiting times; lack of awareness of the need for
screening; and language barriers. 15 individuals attended
the workshop, all of whom confirmed that the session
improved their knowledge of breast cancer.
Discussion
Our research showed that Muslim women experience
inequalities in their access to cancer screening. Think
Pink aimed to overcome these barriers by providing a
faith-based, culturally cognizant intervention directly
engaging the community. The limitations of our research
were a lack of participant data pre and post-workshop
Furthermore, the Google Form survey had minimal
language options which may not have covered the full
spectrum of languages spoken by this population.
We recommend that Think Pink be replicated in other
locations, accompanied by stringent data collection for
continual improvement and targeting of more barriers. At
the macro level, there needs to be greater dialogue and
education between policymakers, healthcare
professionals and Muslim women, to enable better
engagement for stigmatised health issues, and to
empower patients with greater autonomy
References
- Christie-de Jong F, Kotzur M, Amiri R, Ling J,
Mooney JD, Robb KA. Qualitative evaluation of a
codesigned faith-based intervention for Muslim
women in Scotland to encourage uptake of breast,
colorectal and cervical cancer screening. BMJ Open
2022;12(5).
Figures