Abstract
The Human Papillomavirus (HPV), is described as the killer of young women; causing cervical cancer in women younger than 50 years old. Gardasil-9 the vaccine offered by the NHS to children as young as 12-13 years of age, could help protect against nine strains of HPV; two of which can cause anogenital warts and five strains that are oncogenic. The contention that may arise concerning providing consent to HPV vaccines is the notion that offering vaccines at such a young age may lead to early sexual activity. Parents and HCPs may feel that offering the vaccine is a form of promoting a promiscuous society This paper examines the spread of HPV and the need for the vaccine at an early age. HPV vaccination programmes from Muslim-majority countries are also taken into account. The concept of ‘assisting’ is also explored in light of the Holy Qur’an.
Human Papillomavirus(HPV)
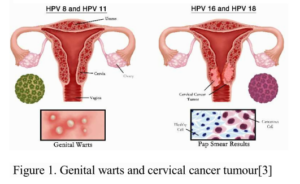
The Human Papillomavirus (henceforth HPV); induce exophytic lesions of the skin and mucous membranes. Over 150 types of HPVs exist which can be categorised by their oncogenicity (ability to cause cancer, especially cervical). More than 40 types of HPV cause anogenital warts (see Figure 1 below). The virus is extremely common and almost all sexually active men and women contract some strains of the virus at some point in their lives [1].
A person’s immune system, however, will naturally clear infections. Other infections, nevertheless, could remain in the body for many years before they cause damage. Two types, HPV 6 and 11, are known to cause anogenital warts whereas 14 types of HPV are known to cause cancer [2]. A sexually active person carrying HPV could transmit it to their partner through sexual activity.
Non oncogenic HPVs 6 and 11
HPV 6 and 11 are known to cause anogenital warts 90% of the time[4][5]. Although a carrier may not feel any change immediately upon contracting HPV, after many months, they will experience the growth of anogenital warts.
Oncogenic HPVS
14 HPVs ( 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68) are high risk (see Table 1 below). These HPVs cause anogenital cancers; including vaginal, vulvar, penile, and anal cancers [6]. HPVs can also cause head and neck squamous cell carcinomas (HNSCC). The erous oncogenic types are HPV 16 and 18.
, 39, 45, 51, 52, 56, 58, 59, 66, and 68) are high risk (see Table 1 below). These HPVs cause anogenital cancers; including vaginal, vulvar, penile, and anal cancers [6]. HPVs can also cause head and neck squamous cell carcinomas (HNSCC). The two most dangerous oncogenic types are HPV 16 and 18.
The former is responsible for 20% of all HNSCC [7]. Subsets of HNSCC include oral cavity SCC (OCSCC), oropharyngeal SCC (OPSCC), laryngeal SCC (LSCC) and paranasal sinus cancer [8][9]. HPV 16 is responsible for causinging almostalmost 90%90% ofof OPSCC and is prevalent in males [10]. According to the WHO, in women from low-to-middle-income countries worldwide, HPVs have caused 85% of cervical cancer cases [11].
HPVs 16 and 18 and Cervical Cancer
Two extremely dangerous types of HPVs are 16 and 18, which collectively cause 70% of precancerous cervical lesions and cervical cancer (henceforth CC) worldwide [12][13][14][15].. These two viruses are also responsible for most other HPV-induced anogenital cancers [16]. In Europe, CCs caused by HPV 16 and 18 amount to 75%; and in the UK, 80%. In the UK annually, CC kills around induced anogenital cancers [16]. In Europe, CCs caused by HPV 16 and 18 amount to 75%; and in the UK, 80%. In the UK annually, CC kills around 900 women [17].
With regards to CC, the estimated number of new cases worldwide is approximately 530,000, along with an estimated 270,000 deaths annually [18]. Accordingly, CC is considered to be the fourth most common cancer in women worldwide [19]. However, in terms of age, CC is the most common cancer among women who are 15 to 34 years old [20]. As such, CC mainly kills young women – with 62% of cases occurring in women who are younger than 50 years old [20]. Besides HPVs 16 and 18, types 31, 33, 45, 52 and 58 (see Table 1 above) cause an additional 15% of CCs. Like the gradual emergence of genital warts caused by HPV, CC caused by HPV can also take many years to emerge.
Living as HPV Positive or with cervical cancer
Sexual life can be negatively impacted by HPV-related infections [21]. The impact of HPV infection on women could be devastating physically, sexually, socially, and mentally. Physically, the infection would mainly affect the vulva and cervix. Consequently, physical changes could interfere with intimate relationships and sexual enjoyment may decrease [22][23][24]. Socially, the patient would require repeated tests and treatments. Moreover, social stigma may arise with regard to trust in marital relations. Such impact from various dimensions would harm the patient’s mental health; the patient’s physical health is likely to impact pregnancy plans. Repeated exposure to tests, could lead to feelings of vulnerability, shame, and in terms of femininity, low self esteem.
Gardasil -9
Three vaccines have been developed for protection against HPV infections (see Table 1); these include: a) Cervarix bilavent vaccine, which protects against HPV 16 and 18, b) Cervarix and Gardasil Quardavalent vaccines which protect against HPV6, 11,16 and 18 and c) Gardasil-9, which protects against the following nine strains: oncogenic strains 16 and 18 as well as 31, 33, 45, 52, 58 along with protection against non-oncogenic strains 6 and 11.
HPV vaccines have been monitored and are concluded as safe and having high efficacy in females and males [25]. Additionally, although Gardasil-9 does not treat established HPV infections, it could still protect against other strains and also protect against infection at different mucosal sites [25].
Efficacy of Gardasil-9 at ages 12-13
HPV infections are usually found on the fingers, hands, mouth and genitals and can be spread by any skin-to-skin contact. Therefore, the virus can be spread during any kind of sexual activity, including touching. Although genital HPV is spread through intimate skin-to-skin contact during sexual activity, HPV strains that infect the mouth and throat can be passed on through kissing. An individual can have a genital virus for many years before any symptoms appear. As such, an individual might not be aware for many years that their partner is a carrier. The HPV vaccine is thus most effective when received before coming into contact with HPV i.e. around the ages of 12-13 before becoming sexually active [26].
The NHS information on HPV vaccines states that it is ‘given as 2 injections into the upper arm spaced at least 6 months apart. In school Year 8, girls and boys aged 12 and 13 are routinely offered the first dose of the HPV vaccine free of charge. The second dose is also free and is offered 6 to 24 months after the first dose [27]. Moreover, the vaccination is free on the NHS until one’s 25th birthday for girls born after 1 September 1991 and boys born after 1 September 2006. Beyond these conditions, patients requiring HPV vaccines would have to pay for each injection privately.
HPV Vaccination in Muslim majority countries
Given the harrowing statistics on HPV, the WHO’s global strategy for the elimination of cervical cancer has led to over 100 countries, including Muslim countries having introduced HPV vaccination [28]. Indonesia and Bangladesh, for instance, are offering vaccines at doctor offices, community health clinics, school-based health centres, and health departments. [29]
In Malaysia [30], Gardasil was made available for private use in 2006, and Cervarix in 2010, for females
aged 9 to 40 years [31][32]. The National HPV Immunization Program was led by the Ministry of Health (MOH). The program aims to vaccinate about 250,000 school girls aged 13 years old every year with a goal to prevent 27,000–32,200 cases of cervical cancer by the year 2070 [33]. The success of the vaccine programme in Malaysia appears to be the strong triangulated collaboration of the MOH, the Ministry of Education, and importantly, the Fatwa council. JAKIM declared that not only were the HPV vaccines safe and permissible but that, from a Shariah viewpoint, they were required [34][35][36][37].
In the Middle East, the Saudi Food and Drug Administration approved the Bivalent vaccine (Cervarix and Quadrivalent vaccine (Gardasil) in 2010 for females aged 11 to 26 years. [38] Moreover, the vaccines were made available to males as an option and as part of the routine vaccine programme for females [38]. Vaccination is accommodated at private hospitals and clinics along with a few major hospitals as well as paediatric clinics [38]. Furthermore, parental consent has been found to be high [39]. A study in the UAE by Ortashi et al. [40] found that ‘80% of those who had heard about HPV vaccination were willing to be vaccinated themselves, and 87% would recommend vaccination to relatives and friends’. The HPV vaccine is given to females prior to age 15.
The main challenge with regard to HPV uptake in Libya and UAE where exist HPV programmes exists appears to be financial constraints [ [41]]. Likewise, the Iranian government has not been able to implement an immunisation programme due to the HPV vaccines not being cost-effective [42][43]. Many other EMR countries have also been facing economical challenges, however HPV vaccines can be received in the private sector[44]. Despite, Malaysia’s successful vaccination programme, the COVID-19 pandemic led to a halt in the national school vaccination programme in 2020 and 2021. The disruption resulted in about 225000 females aged 13 years old missing their vaccination [45]. Resultantly, many parents have been unable to pay for their children’s HPV vaccines due to extra costs [45].
Another factor which Heffernan et al. attribute to the reluctance toward sexual and reproductive health in the Middle Eastern North Africa (MENA) region is the notion that ‘cultural normative values toward pre-marital sexual behaviour being forbidden in the Islamic faith and associated family dishonour and shame, and stigma with sexuality discourses’ [46]. However, studies have shown that adolescent sexual activity is already existent and increasing in young Muslims aged 14-17 [13][47] Irrespective of Shariah guidelines, such findings reveal the high risk of HPV morbidities. Additionally, some HCPs might also feel that by promoting the vaccine, they are tacitly approving non-Shariah compliant behaviour [13].
HPV Vaccination in the UK
According to the 2015 report from Public Health England, since vaccines were introduced, HPV infections in young women have significantly decreased. To elaborate, in the UK, prior to the start of the vaccination, HPV was the most common sexually transmitted infection. The HPV immunisation programme in England has contributed to almost eradicating cervical cancer in women born since Sept 1995 [48]. As such, the HPV vaccination programme is having an impact on reducing the number of CCs in the future.
Contentions among British Muslims: Promotions of a promiscuous society
One fear related to the HPV vaccine for some HCPs Muslim parents is that the NHS vaccination programme might encourage sexual activity exo-nikah (which includes pre-marital and extra-marital). From a Shariah viewpoint, sexual activity is permitted only intus-nikah meaning within the institution of marriage. In England and Wales, according to the Marriage and Civil partnership Act 2022, which came into effect in February 2023, the age of marriage and civil partnership has been raised to age 18. With the HPV vaccines being offered at early as age 12, the fear in some members of the British Muslim community might be the notion that the youth may take advantage of the vaccine to engage in sexual activity exo-nikah. Even prior to the law change, one study revealed that 20% of Muslim Pakistani mothers declined the vaccination on religious grounds [13]. In Pakistan, due to a lack of an HPV vaccination programme, 68.6 million women are at risk of CC [49]. If a programme was to be introduced in Pakistan, over 133,000 cervical cancer cases could be prevented [50]. In religious communities, some mothers perceived the religious notion of abstinence from pre-marital sex as grounds for not requiring the vaccine [51][52][53][54]. On the other hand, according to a survey study in Lahore, Pakistan, 50 – 60% of the respondents mentioned that they would get the vaccine if it was recommended by their physician [55].
Another reason for refusing the vaccine – found among Jewish communities and a reason that could likely be the case in Muslim ones – is the lack of perceived risk of HPV-related disease because of circumcision and abstinence from sex before marriage [52]. The solution is, therefore, believed to be simply refraining from sexual activity until marriage. Such an approach appears to be based on good faith that one’s partner(s) will also not engage in any sexual activity nor will they have contracted HPV orally.
Returning to the belief that vaccination is tacit approval for exo-nikah sexual activity, the contention appears to be rooted in the Qur’an. Verse 5:2, ‘Help one another in birr and taqwa but do not help one another in ithm and udwan’. From a linguistic perspective, the general translation of ithm is given as ‘sin’ (52 English translations). Birr is translated as ‘righteousness’ (35) or ‘good’ (20) and is explained by Qur’anic commentators to be antonymous in the verse to ithm. Likewise, taqwa translated as ‘piety’ (39) and is explained to be antonymous in the verse to udwan, which was found to be translated in a number of ways including ‘transgression’ (34), ‘aggression’ (23), ‘enmity’ (15), and ‘hostility’ (15).
Through the lens of Islamic jurisprudence, however, ithm is applied to an act that is regarded as intrinsically sinful such as stealing and murder. On the other hand, udwan is when actions that are permitted but are done beyond their permitted limits and boundaries are seen as ‘transgression’. For instance, eating and drinking are permitted, however, to have a fatal diet would be considered udwan. Likewise, sexual activity is permitted intus-nikah whereas sexual activity exo-nikah is considered another form of udwan.
Moreover, the context of verse 5:2 is explained by Tabari [56] (d.839) and Tusi [57] (d.1067) to refer to a case during the time of the Prophet (peace be upon him) when a group of Medinites collaborated to exact revenge on a thief. An individual by the name of AlHutam bin Hind Al-Bakri had travelled to visit the Prophet in Medina under the pretence of inquiring about Islam. However, on leaving Medina, he raided cattle belonging Medinites and on reaching Yemen, he slaughtered the cattle and profited immensely from sales. Al-Hutam then used the profits to purchase a large amount of merchandise to sell at the upcoming Hajj. The Muslims who were outraged by his audacity wanted to arrest and take Al-Hutam to account. However, Al-Hutam sought refuge within the sacred vicinity. Given the sanctity of the time and place, the Qur’an highlights that killing the thief would be ithm and to support one another in arresting him in the sacred vicinity or forcefully removing him therefrom, would be udwan.
As such, a significant contextual difference arises between offering HPV vaccines and the incident referred to in the Qur’an. The latter prevents Muslims from carrying out a process which involves compromising key Islamic values, albeit to establish justice, whereas offering HPV vaccines does not appear to violate any value. The hesitancy around the HPV vaccine is then based on fear of abusing the vaccine programme; which is beyond the remit of HCPs.
A key Islamic jurisprudential maxim to bear in mind is
‘al-umour bi-maqasidiha’ meaning ‘Matters are
determined by their purpose [58]. Another relevant
maxim is ‘al-ebratu bi-siyagh al-uqoud aw bi-ma’anih
meaning ‘Matters are to be considered based on linguistic
representations and their meanings’ [59]. The purpose of
offering HPV at a young age, as stated by the NHS, is to
protect against HPV before children come into skin to
skin contact with an individual who has HPV.
Irrespective of Shariah guidelines promoted in culture,
child sexual abuse is a reality that must not be
overlooked.
Offering HPV vaccines does not amount to helping in
ithm. The HCP, offering the vaccine to a child, intends
safety. The HCP’s responsibility is to prevent harm.
Furthermore, the patient’s intentions would unlikely be
verbalised i.e. that the patient would state that they would
like the HPV vaccine so that they could engage in sexual
activity exo-nikah. Additionally, the Qur’an clarifies that
one shall not bear the burden of another’s sin [60]. The
Qur’an, therefore, places no blame on the HCP for
providing sincere clinical support to prevent harm.
Moreover, according to Islamic theology, sexual activity
exo-nikah is a matter that is deferred to Allah for
judgement, whereas providing clinical support is
regarded as an honourable service to His creation.
Supporting HPV vaccines is also not the same as
euthanasia or abortion, because the latter two cases
involve taking a life which directly falls under ithm. In
the context of HPV vaccines, ithm would be to engage in
sexual activity exo-nikah post-vaccination whereas
verbally encouraging the act post-vaccination would be
considered udwan.
Furthermore, Shariah law prioritises halal over haram.
The recommended Sharia approach is to base decisions
on the idea that Muslims will opt for halal – as that is
what they have subscribed to willingly. According to the
Qur’an and hadith literature, dhann (suspicion) is
criticised as the worst basis for making decisions [61]. As
such, the central idea with regard to HPV vaccines is that
Muslims would be able to enjoy a healthier life mentally,
sexually, physically, socially and spiritually.
Fewer cases of HPV would need to be disclosed prior to
marriages and couples would be able to enjoy safe halal
sexual relations intus-nikah. Moreover, in unfortunate
cases of sexual abuse or where a spouse did not disclose
carrying HPV, the victim would have a better chance of
not contracting HPV.
Discussion
Before British Muslims refuse to receive HPV Vaccine
or decline on behalf of children, some considerations are
important.
From a moral perspective, whilst providing pastoral care
is primarily the role of the ulama, an existing illness still
requires management by HCPs. Treating medical
conditions are viewed in Shariah as a form of ihsan
meaning kindness. Secondly, although an individual may
abstain from sexual activity exo-nikah, the vaccine would
protect them from contracting HPV should their partner
be a carrier. The symptoms of HPV also include
anogenital warts, which could result in the patient
suffering from poor mental health and low self-esteem
Moreover, the vaccine could save individuals from social
stigma.
In terms of costs, British Muslims are fortunate to have
access to Gardasil-9. At the time of writing, this vaccine
was unavailable in many low income and middle-income
countries that are not eligible for support from Gavi [62].
As discussed, even in Muslim countries like Malaysia
and Iran, parents and the government have faced
economical challenges.
Perhaps a strong point to consider is the fact that a
country like Saudi Arabia promotes vaccination despite
its stringent regulations to prevent sexual activity exo
nikah. For instance, culturally, such behaviour is strongly
discouraged from a religious viewpoint. Couples would
not be permitted to make reservations at a hotel without a
marriage certificate. Even when couples intend to marry,
a blood test is required to detect genetic and infectious
illnesses. Such measures contribute to decreasing sexual
activity and thereby, the spread of STIs, yet HPV
vaccination is encouraged. In the UK, such stringent
measures to prevent sexual activity are not in place, nor
are blood tests for marriage purposes a requirement
culturally or legally. As such, British Muslims ought to
strongly consider receiving the HPV vaccination for their
protection and perhaps, even consider blood tests for
marriage purposes.
Conclusion
HPV is known to cause anogenital warts and cervical
cancers. Many strains of the virus exist, however the
Gardasil-9 vaccine helps to protect against nine strains of
which five are oncogenic. Living with HPV can have a
negative impact physically, sexually, mentally, and
socially. The most effective period to receive the vaccination is around 12-13 years of age i.e. prior to
becoming sexually active. Offering the vaccine to
individuals is to promote health and safety and is a form
of assisting in public welfare.
A collaboration of medical experts and Muslim jurists is
key to addressing patient concerns. Educational sessions
could be held in Mosques, Islamic seminaries, and
community centres during Ramadan, Hajj, and marriage
seasons. Alternatively, mobile vaccination vehicles could
be stationed where British Muslims gather. Sessions
could be tailored and delivered in languages understood
by patients and influential members of communities to
address myths and misconceptions.
HCPs and faith leaders need to educate the public on the
fact that Gardasil-9 does not protect individuals against
other types of HPV types (see Table 1). Neither is the
vaccine a form of contraception nor does it protect
against other infections that could spread during sex,
such as AIDS, chlamydia, gonorrhoea, and syphilis.
Likewise, common warts can still be caused by HPV
types 1, 2, and 4; planter warts by types 1, 2, and 4;
anogenital warts by types 6, 11, 42, 43, 44, 55 and more;
epidermodysplasia verruciformis by more than 15 strains;
oral focal epithelial hyperplasia by types 13 and 32; and
oral papillomas by types 7 and 32 [63]. In line with the
UN joint global programme on CC prevention and
control [12], cancer screening also needs to be promoted
given that the only type of HPV-related cancer with a
recommended screening test is CC.
In addition to grassroots efforts to promote better health
care, HCPs and Muslim jurists could collaboratively
author ‘medical fatwas’ [64] on HPV to promote an
informed and unified stance. Importantly, given that HPV
causes cervical cancer in young women, female
perspectives on this matter are crucial.
Notes
Malay: Jabatan Kemajuan Islam Malaysia – the federal
government agency in Malaysia that administers Islamic
affairs in Malaysia.
b The technical term for ‘marriage’ in Shariah is law is
nikah comprising of terms and conditions.
References
- NHS UK. Human papillomavirus (HPV) [Internet];
2022, May 27 [cited 2023, Feb 8]. Available
from:https://www.nhs.uk/conditions/human-papilloma-
virus-hpv/ - Patel, H., Wagner, M., Singhal, P. and Kothari,
S.Systematic review of the incidence and prevalence of
genital warts. BMC Infectious Diseases. 2013, 13(39), 1
14. - Walls, S. Human Papillomavirus (HPV) Strains 6 and
11 and Strains 16 and 18. Embryo Project Encyclopedia
[Internet]; 2021, Apr 6 [cited 2023, Feb 8]. Available
from:http://embryo.asu.edu/handle/10776/13250 - Greer, C.E., Wheeler, C.M., Ladner, M.B., Beutner,
K., Coyne, M.Y., Liang, H., Langenberg, A., Yen, T.S.
and Ralston, R. Human papillomavirus (HPV) type
distribution and serological response to HPV type 6
virus-like particles in patients with genital warts. Journal
of clinical microbiology. 1995, Aug, 33(8), 2058 - Sturegård, E., Johansson, H., Ekström, J., Hansson,
B-G., Johnsson, A., Gustafsson, E., Joakim, D. and Ola,
F. Human Papillomavirus Typing in Reporting of
Condyloma. Sexually Transmitted Diseases. 2013, Feb
40(2), 123-9. - de Martel, C., Plummer, M., Vignat, J. and
Franceschi, S.Worldwide burden of cancer attributable to
HPV by site, country and HPV type International
Jounrnal of Cancer. 2017, 141(4) , 664-670 - Ndiaye, C., Mena, M., Alemany, L., Arbyn, M.,
Castellsagué, X., Laporte, L., Xavier Bosch, F. X., Silvia
de Sanjosé, S. and Helen Trottier, H.
mRNA, and p16INK4a detection in head and neck
cancers: a systematic review and meta
Oncology. 2014, 15(12), 1319 - Syrjanen, K., Syrjanen, S. and Pyrhonen, S.
papilloma virus (HPV) antigens in lesions of laryngeal
squamous cell carcinomas. ORL; Journal of Oto
Laryngol Related Specialties. 1982, 44(6), 323 - Syrjanen, K., Syrjanen, S., Lamberg, M., Pyrhonen,
S. and Nuutinen. J.
immunohistochemical evidence suggesting human
papillomavirus (HPV) involvement in oral squamous cell
carcinogenesis. International Journal of Oral Surger
1983, 12(6), 418-24. - Jamal, Z. and Anjum, F.Oropharyngeal Squamous
Cell Carcinoma. StatPearls. 2022. - Wilailak, S., Kengsakul, M. and Kehoe, S.
Worldwide initiatives to eliminate cervi
cancer.International Journal of Gynecology & Obstetrics
2021 Oct, 155(S1), 102-6. - Buang, S.N., Ja’afar, S., Pathmanathan, I. and Saint,
V. Human papillomavirus immunisation of adolescent
girls: improving coverage through multisectoral
collaboration in Malaysia. BMJ. 2018, Dec 7, k4602. - Hamdi, S.The impact of teachings on sexuality in
Islam on HPV vaccine acceptability in the Middle East
and North Africa region. Journal of Epidemiology and
Global Health. 2018, 7(S1), S17-S22. - Lowy ,D.R. and Schiller, J. T.Prophylactic human
papillomavirus vaccines. Journal of Clinical
Investigation. 2006, 116(5), 1167-73 - Muñoz ,N., Bosch, F.X., Castellsagué, X., Díaz, M.,
de Sanjose, S., Hammouda, D. Shah, K. V. and Meijer,
C.J.L.M.Against which human papillomavirus types shall
we vaccinate and screen? the international perspective
International Journal of Cancer. 2004, Apr 12, 111(2),
278-85. - Gao, G. and Smith, D.I.Human Papillomavirus and
the Development of Different Cancers. Cytogenetic and
Genome Research. 2016, 150(3-4), 185-93. - Vaccine Knowledge. HPV (Human Papillomavirus);
What are the symptoms? [Internet]; 2019, Oct 18 [cited
2023, Feb 8]. Available
from:https://vk.ovg.ox.ac.uk/hpv#What-are-the-
symptoms - Tota, J.E., Chevarie-Davis, M., Richardson, L.A.,
deVries, M. and Franco, E.L.Epidemiology and burden
of HPV infection and related diseases: Implications for
prevention strategies. reventive Medicine. 2011, Oct
53(S1), S12-21. - WHO. Cervical cancer [Internet]; N.D. [cited 2023,
Feb 8]. Available from:https://www.who.int/health
topics/cervical-cancer - Vaccine Knowledge. HPV (Human Papillomavirus);
Key disease facts [Internet]; 2019, Oct 18 [cited 2023,
Feb 8]. Available from:https://vk.ovg.ox.ac.uk/hpv#Key
disease-facts - Qaderi, K., Germmaych, M., Mirmolaci, S.T.,
Farnam, F. and Hasani, S.S.
Iranian Women with Human Papillomavirus’ Sexual
Life. The Journal for Nurse Practitioners. 2021, Nov
17(10), 1261-6. - Caruso, S., Bruno. M.T., Cianci, S., Di Pasqua, S.,
Minona, P. and Cianci,A. Sexual behavior of women
with diagnosed HPV. Journal of Sex & Marital Therapy.
2019, 45(7), 569-73. - Ferenidou, F., Salakos, N., Vaidakis, N., Paltoglou,
G., Bakalianou, K., Papadimitriou
The impact of HPV diagnosis on women’s sexual and
mental health: preliminary findings. Clinical and
Experimental Obstetrics & Gynecology. 2012, 39(1), 79
82. - Clarke. P., Ebel, C., Catotti, D.N. and Stewart,
S.The psychosocial impact of human papillomavirus
infection: implications for health care providers
International journal of STD & AIDS. 1996,7(3), 97-200 - Diana, G. and Corica, C. Human Papilloma
vaccine and prevention of head and neck cancer, what is
the current evidence?. Oral Oncology. 2021, 115,
105168. - Moro. P.L., Zheteyeva, Y., Lewis, P., Shi, J., Yue,
X., Museru, O.I. and Broder, K.
human papillomavirus vaccine (Gardasil®) in pregnancy:
Adverse events among non
Vaccine Adverse Event Reporting System, 2006
Vaccine. 2015, 33(4), 519-22. - NHS UK. HPV vaccine overview [Internet]; 2019,
May 10 [cited 2023, Feb 8]. Available
from:https://www.nhs.uk/conditions/vaccinations/hpv
human-papillomavirus-vaccine/ - WHO. Global strategy to accelerate the elimination
of cervical cancer as a public health problem [Internet];
2020, [cited 2023, Feb 8]. Available
from:https://apps.who.int/iris/handle/ - LaMontagne, D.S., Bloem, P.J.N., Brotherton,
J.M.L., Gallagher, K.E., Badiane, O. and Ndiaye,
C.Progress in HPV vaccination in low
middle-income countries. International Journal of
Gynaecology & Obstetrics. 2017, 138(S1), 7 - Muhamad, N.A., Buang, S.N., Jaafar, S., Jais, R.,
Tan, P.S., Mustapha, N., Lodz, N.A., Aris, T., Sulaiman L.H. and Murad, S.Achieving high uptake of human
papillomavirus vaccination in Malaysia through school
based vaccination programme. BMC Public Health.
2018, 18(1). - U.S. Food and Drug Administration. Gardasil
[Internet]. 2023, Mar 6 [cited 2023, Mar 6]. Available
from:https://www.fda.gov/vaccines-blood
biologics/vaccines/gardasil - U.S. Food and Drug Administration. Cervarix
[Internet]. 2019, Oct 10 [cited 2023, Feb 8]. Available
from:https://www.fda.gov/vaccines-blood
biologics/vaccines/cervarix - Keane, A., Ng, C.W., Simms, K.T., Nguyen, D.,
Woo, Y.L., Saville, M. and Canfell, K.
cervical cancer elimination in Malaysia: evaluation of the
impact and cost-effectiveness of human papillomavirus
screening with self-collection and digital registry sup
International Journal of Cancer. 2021, 149(12), 1997
2009 - Isa, N.M., Baharuddin, A., Man, S., Chang,
L.W.Bioethics in the Malay-Muslim Community in
Malaysia: A Study on the Formulation of Fatwa on
Genetically Modified Food by the National Fatwa
Council. Developing World Bioethics. 2014, 15(3), 143
151. - Anon. The Ruling on Using Human Papilloma Virus
Vaccine (HPV); The 92th Muzakarah (Conference) of the
Fatwa Committee National Council of Islamic Religious
Affairs Malaysia held on 15-17 December 2010 [pdf];
2011, Apr 4 [cited 2023, Feb 8]. Available
from:http://irep.iium.edu.my/16091/1/HALAL_PHARM
ACEUTICAL-2011.pdf - Fine, P.E.M. and Griffiths, U.K.Global poliomyelitis
eradication: status and implications. Lancet. 2007,
369(9570), 1321-1322. - Habib, A.G., Abdulmumini, M., Dalhat, M.M.,
Hamza, M. and Iliyasu, G.Anti-retroviral therapy among
HIV infected travelers to Hajj pilgrimage
Travel Medicine. 2010, 17(3), 176-181. - Noor, U.M.M. Bayan Linnas Siri Ke
Kewajiban Mengambil Vaksin Mengikut Jadual
Imunisasi Kebangsaan Daripada Perspektif Islam
[Internet].2019, Feb 18 [cited 2023, Feb 8]. Available
from:https://muftiwp.gov.my/ms/artikel/bayan
linnas/3129-bayan-linnas-siri-ke-166-kewajiban - Hussain, A.N., Alkhenizan, A., McWalter, P., Qazi,
N., Alshmassi, A., Farooqi, S. and Abdulkarim,
A.Attitudes and perceptions towards HPV vaccination
among young women in Saudi Arabia
& Community Medicine. 2016, 23(3), - Altamimi, T.Human papillomavirus and its
vaccination: Knowledge and attitudes among female
university students in Saudi Arabia
Medicine and Primary Care. 2020, 9(4), 1849 - Ortashi, O., Raheel, H. and Shalal, M.
of Human Papilloma Virus Vaccination among Women
in the United Arab Emirates
Cancer Prevention. 2014, 15(5 - EMRO WHO.Meeting of the Eastern Mediterranean
Regional Technical Advisory Group on immunization
East Mediterranean Health Journal. 2018, 24(6), 604 - Sargazi, N., Takian, A., Yaseri, M., Daroudi, R.,
Motlagh, A. G., Nahvijou, A. and Zendehdel, K.
preferences and willingness
papillomavirus vaccines in Iran: A discrete choice
experiment study. Preventive Medicine Reports. 2021,
23, 101438. - Yaghoubi, M., Nojomi, M., Vaezi, A., Erfani, V.,
Mahmoudi, S., Ezoji, K., Zahraei, S. M.,
Moradi-Lakeh, M.Cost-effectiveness analysis of the
introduction of HPV vaccination of 9
Iran. Value in Health Regional Issues. - Sargazi, N., Takian, A., Daroudi, R., Nahvijou, A.,
Yaseri, M., Ghanbari Motlagh, A. and Kazem Zendehdel,
K.Cost-Benefit Analysis of Human Papillomavirus
Vaccine in Iran. Journal of Prevention. 2022, 43(6), 841
57. - Rao, S.R., Kampan, N., Chew, K.T., and Shafiee,
M.N.The impact of the COVID
national HPV immunization program in Malaysia
Frontiers in Public Health. 2022, 10 - Heffermnan, M., Alzaabi, O. and Arulappan, J.
Addressing disparities in HPV vaccination among
culturally diverse populations
approach [Internet]; 2022, Oct [cited
Available
from:https://www.hpvworld.com/articles/addressing-disparities-in-hpv-vaccination-among-culturally
populations-a-socioecological-approach/ - Gamaoun, R.Knowledge, awareness and
acceptability of anti-HPV vaccine in the Arab states of
the Middle East and North Africa Region: a systematic
review. Eastern Mediterranean Health Journal. 2018,
24(6), pp.538-48. - Falcaro, M., Castañon, A., Ndlela, B., Checchi, M.,
Soldan, K., Lopez-Bernal, J., Elliss-Brookes, L. and
Sasieni, P.The effects of the national HPV vaccination
programme in England, UK, on cervical cancer and grade
3 cervical intraepithelial neoplasia incidence: a register
based observational study. The Lancet, 398(10316),
2084-92. - Shamsi, U., Anwar, A. and Samad, Z. Time for
Reintroducing HPV Vaccine in Pakistan for Primary
Prevention of Cervical Cancer. Journal of College of
Physicians and Surgeons Pakistan [Internet].
[cited 2023, Feb 8]. Available
from:https://www.jcpsp.pk/article-detail/ptime
reintroducing-hpv-vaccine-in-pakistan-for
prevention-of-cervical-
cancerorp#:~:text=The%20government%20of%20Sindh
%2C%20Pakistan - Portnoy, A., Abbas, K., Sweet, S., Kim, J.J. and Jit,
M.Projections of human papillomavirus (HPV)
vaccination impact in Ethiopia, India, Nigeria and
Pakistan: A comparative modelling study
Health. 2021, 6(11), e006940. - Brabin, L., Roberts, S.A., Farzaneh, F. and
Kitchener, H.C.Future acceptance of adolescent human
papillomavirus vaccination: A survey of parental
attitudes. Vaccine. 2006, 24(16), 3087‐3094. - Gordon, D., Waller, J. and Marlow, L.A.V.
to HPV vaccination among mothers in the British Jewish
community: Reasons for accepting or declining the
vaccine. Vaccine. 2011, 29(43), 7350‐6. - Katz, M.L., Reiter, P.L., Heaner, S., Ruffin, M.T.,
Post, D.M. and Paskett, E.D.
vaccine among women, parents, commun
healthcare providers in Ohio Appalachia
27(30), 3945‐52. - Marlow, L.A., Wardle, J., Forster, A.S. and Waller,
J.Ethnic differences in human papillomavirus awareness
andvaccine acceptability. Journal of Epidemiology &
Community Health. 2009, 63(12), 1010 - Khan, T.M., Buksh, M.A., Rehman, I.U. and
Saleem, A.Knowledge, attitudes, and perception towards
human papillomavirus among university students in
Pakistan. Papillomavirus Research. 2016, 2, 122 - Bin Jareer, M. Jami’ al-bayan fi ta’weel al-Qur’an
Beirut, Lebanon: Dar Al-Kot - Al-Tusi, M.H. Al-Tibyan fi tafsir al-Quran
- Al-Subki, A.A. Al-Ashbah wa’n nadha’ir. Beirut,
Lebanon: Dar Al-Kotob Al-ilmiyah; 1991. - Al-Suyuti, A. Al-Ashbah wa’n nadha’ir. Beirut,
Lebanon: Dar Al-Kotob Al-ilmiyah; 1991. - The Holy Qur’an, chapter 35: verse
- Al-asbahi, M. Al-Mu’atta Imam Malik; Kitab husn
al-khuluq; bab ma ja’a fi’l muhajara. Istanbul, Turkey;
Dar al-Lubab; 2019. - Trimble, C.L. andTrimble, E.L. HPV vaccines:
when one plus one equals three. The Lancet Global
Health. 2022, 10(10), e1373– - Human Virology at Stanford. Human
Papillomavirus; What are the diseases induced by HPV?
[Internet]. N.D. [cited 2023, Mar 12). Available
from:https://virus.stanford.edu/papova/HPV.html - Maravia, U. Now is the time for a unified medical
fatwa. Journal of the British Islamic Medical Association.
2021, 7(3), 85-86.