Abstract
The NHS is struggling to retain health care providers, a notion that could be described as Drexit, as a
consequence of Brexit. One solution to retaining health care providers is to welcome diversity by exploring
Islamic medical ethics. British Muslims form a significant portion of the NHS. A look into the legacy of
Muslims and health care may help to reduce Islamophobia and appreciate what inspires and motivates Muslim
health care providers to contribute to the NHS. This legacy can be explored by visiting the way bimaristans,
which were hospitals largely funded by Muslim philanthropists, operated in the Middle Ages. By understanding
the way bimaristans helped to develop ancient medicine and the way they influenced European hospitals can
help to shed light on Islamic medical ethics. Importantly, Islam promotes an attitude of well-being for patients
and teaches health care providers to remain modest and resilient throughout their careers whilst always
endeavouring to improve the provision of health care.
Introduction
The NHS has certainly become a world-renowned and admired health service. Among the NHS’ greatest achievements include arguably its provision of care based on need and free health care for all as a basic human
right. Free care by the NHS is a commendable aspect of health care. Free care removes the fear for patients of
how they would pay for their treatment. Furthermore, free care allows health care providers to focus on their
patients’ health rather than engage in financial discussions about the treatment. The strength of the NHS lies in its withstanding the numerous restructures and adaptations to innovation to meet the demands of an ever-growing and ageing population. Additionally, the NHS continues to meet the needs of the diverse cultural needs of patients [1].
Nevertheless, health care providers continue to face two main challenges a) for doctors to maintain a strong trusting relationship with patients and b) for the NHS to retain health care providers. In this article, we examine, from the Middle Ages, the organisation and setup of Muslim hospitals, better known as bimaristans, to explore a range of traditional approaches based on Islamic medical ethics. The bimaristans were known to
welcome staff diversity including multi-ethnicity and multi-faith perspectives to address everyday problems.
Such diversity attracted health care providers and patients. Additionally, this ecumenical approach also
attracted philanthropists to fund the bimaristans to acquire the latest medical equipment, instruments, and
services. We also explore, in this article, the way Islamic medical ethics influenced and inspired medical practice
in Europe.
As the NHS is a patient-centred service, by revisiting the way bimaristans operated, insight could be gained into
the traditions, norms, values, and needs of Muslim patients and health care providers. Stakeholders could
then apply this knowledge to accommodate better the needs of a diverse range of health care providers and
patients.
Bimaristans inspired Muslim health care providers to take up the career by appealing to the spiritual reward of
saving lives being equal to saving humanity, as described in the Holy Qur’an. Muslim physicians also viewed
illnesses as a test of patience rather than a curse and believed that the body and soul were both possible to
save. Moreover, based on Prophet Muhammad’s (Peace be upon him) vision, Muslim philanthropists supported
bimaristans through generous donations to serve as peacemakers.
2.1 Qur’anic perspective on medicine as a career
In Islam, humans are believed to have the important role of exercising God’s will on Earth through justice and
kindness. Each individual plays a different role in contributing to the many complex systems that lead to
creating a harmonious civilisation. Prophet Muhammad taught that everyone should commit to their work
because the inspiration to work comes from God – to lead a person to their destiny [2][3]. The idea of tawfeeq,
meaning ability, is likewise, an important concept for Muslims. A sufi understanding is that the sense of
responsibility one feels to serve a noble call is ilham meaning inspiration and blessing from God. Likewise,
the notion of khidma meaning ‘service’ and working fi sabil Allah meaning ‘for the sake of Allah’, all promote a
strong Islamic work ethic.
The Qur’an states that ‘If anyone saves a life, it is as if he saves the lives of all mankind’ [4]. As such, Muslim
patients might not only feel the natural need to take care of their health but Islam places a sense of duty on humanity and especially on physicians to take care of the ill. In this way, the physicians may feel a sense of achievement by treating their patients, whereas the patients may feel a sense of wanting to regain their health so that they may continue to serve their calling. Furthermore, the higher objectives of Islamic law, known as the maqasid al-shari’ah, which are based on the Qur’an, include preservation of faith, life, mind, offspring, and wealth [5].
Based on these objectives, the bimaristans ensured that quality health care was provided. At the centre of health care in Islam is the notion of being mindful of one’s purpose and goal in life. With regard to such a calling, Prophet Muhammad reminded people to value five thingsbefore they are lost: youth, good health, financial
stability, leisurely time, and indeed life itself [6]. Based on the Qur’an and the teachings of Prophet Muhammad,
the ethos of a bimaristan could be understood as being a place where physicians felt a strong sense of religious
duty toward their patients [7]. The expectation of healthcare providers appears to have been to seek spiritual
satisfaction more so than to gain only material rewards. The prophetic teachings on taking care of the sick focus
not only on the physically sick but focus also on those facing mental health issues. Likewise, the focus is not
only on city dwellers, but also on being mindful of the sick among the Bedouins, travellers, prisoners, and other
categories of people who are likely to be overlooked and who may have lower life expectancy.
2.2 Attending to the body and faith
A popular belief in Europe during the middle-ages was that certain illnesses were a curse from God. By contrast,
Muslim theologians viewed sickness itself to be a means of atonement. Treating physical symptoms, on the other
hand, was viewed as a noble effort because it restored patients’well-being. Scholars from Prophet Muhammad’s progeny also engaged in changing the mindset of the people towards diseases. Jabir bin Hayyan (d.813), who is regarded as the father of Arab chemistry and one of the founders of modern pharmacy[8], creditsJa’far al-Sadiq (d.765) as the source of his knowledge of chemistry [9].Ja’far’s son Musa al-Kazim (d. 799) would echo the Prophet’s words:
“When a believer falls ill, Allah instructs the scribe to the patient’s left side: “Do not record a single sin against my servant as long as he is in my custody, and in my hold.” And He instructs the scribe to the right: “Write for my servant on his page of good deeds that which you would have recorded for him when he was well.”[10]
Al-Kazim’s son, Ali Al-Rada (d. 818) is credited as having authored the text Al-Risala al-Dhahabiyya, a medical treatise which the Abbasid caliph Al-Mansur (d.775) ordered to have written in gold ink [11].
The teachings of the Prophet Muhammad and his progeny continued to inspire Muslim physicians during
the Abbasid golden era. One notable hadith states that ‘God has appointed a treatment for every disease. So
treat yourselves medically’ [12]. This shift toward attending to the spiritual and physical needs of patients
also meant that to practise medicine, practitioners needed to be qualified in medicine and not that they relied solely on theological knowledge. Prophet Muhammad warned society that ‘should anyone practise medicine without being qualified to do so must be held accountable’ [13]. As such, bimaristans employed only licensed physicians who were held in high esteem and even received high wages. This approach kept the patients safe from quacks and charlatans, as well as from dangerous surgery, which at the time was practised by street barbers.
In this way, physicians at the bimaristans were able to be tend to the spiritual well-being of patients in a manner
similar to the Church. Bimaristans, however, differed by treating the physical symptoms which were explored by
applying and developing Galenic medicine. For instance, leprosy was known to be infectious as detailed by the
Greeks but an illness that was despised in Europe to the point of viewing patients with leprosy as cursed [14].
The bimaristans took a different approach by segregating patients with leprosy humanely. Physicians specialising in treating leprosaria were assigned to treat leprosy. Furthermore, bimaristans had different wards for patients .
suffering from fevers, ophthalmic diseases, dysentery, and psychiatric illnesses. The psychiatric bimaristan in
Baghdad in the 9th century is perhaps the first of its kind [15].
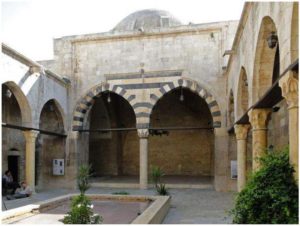
Other renowned psychiatric bimaristans were founded by Ibn Tulun (d. 884) in Egypt in 872 and by the Mamluk
governor Arghun Al-Kamili (image 1 below) in Aleppo in 1354 [16].
Figure 1. BimaristanArghun Al-Kamili
(Aleppo, Syria)[17]
2.3 The Awqaf financing system
During the second medical revolution in Europe towards the end of the 4th century, Christians in the Byzantine Empire had established civilian hospitals in cathedrals [18]. Prophet Muhammad envisioned the next step; a system whereby free health care would be provided to all people irrespective of religion. This vision was actualised when Muqawqis, who administered Egypt on behalf of the Christian Byzantine Empire, sent a physician to Muhammad in Medina. Muhammad instructed the doctor to treat patients gratuitously [19]. Muslims who sought spiritual reward appear to have found the motivation to altruistic rather than focus primarily on receiving material gain for their medical services.
Moreover, Muslim philanthropists funded the bimaristans. The emphasis in the Qur’an to save lives combined with Prophet Muhammad’s charitable approach to health care led to what later developed into bimaristans, a new type of medical-cum-charitable institution, where sick people of all backgrounds could be treated for free [20]. The first mobile dispensary that was set up by Muhammad took the form of a tent at the battle of Khandaq (circa 627), wherein RufaidabintSa’ad, the first female Muslim nurse, treated the wounded [21]
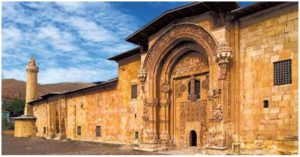
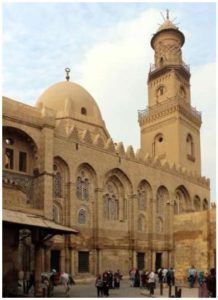
Interestingly, the bimaristans differed from Byzantine hospitals in that the bimaristans were not run by religious establishments nor was supernatural healing practised.Bimaristans were run either by government officials or by philanthropists [22]. A diverse team of physicians of different religions and ethnicities came together to heal the sick. The gratuity led to bimaristans being large elaborate institutions with advanced urban structures, some of which are UNESCO protected sites today (see figures 2 and 3 below). Bimaristans were open to patients of all gender and age groups, belief systems, and to military personnel as well as civilian patients [23].
 Figure 2. Bimaristan Al-Muayyidi(Cairo, Egypt)[24]
Figure 2. Bimaristan Al-Muayyidi(Cairo, Egypt)[24]
Figure 3.Divriği Ulu Cami veDarüşşifası (Divriği Great
Mosque and Hospital, Turkey) [25]
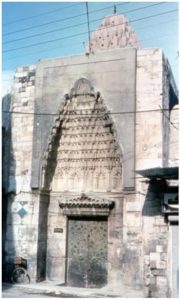
Figuire 4. Bimaristan Al-Mansuri (Cairo, Egypt)[26]
Some bimaristans were extremely large and served as regional primary medical centres. For instance, the
Bimaristan Al-Mansuri (see image 4 above) established in 1248 had 8,000 beds primarily for the people of Cairo
throughout the 15th century [27]. To put into perspective the sheer size of the Bimaristan Al-Mansuri, Northern
Ireland has 41 hospitals with a total of 3,879 beds for a population of 1.89 million [28]. The Bimaristan Al-Mansuripolicy statement read:
The hospital shall keep all patients, men and women, until they are completely recovered. All costs are to be borne by the hospital whether the people come from afar or near, whether they are residents or foreigners, strong or weak, low or high, rich or poor, employed or unemployed, blind orsighted, physically or mentally ill, learned or illiterate. There are no conditions of consideration and payment; none is objected to or even indirectly
hinted at for non-payment. The entire service is through the magnificence of Allah, The Generous One [29].
In 1948, the NHS furthered the idea of free health care when it made health care available to meet the needs of
everyone for free at the point of delivery based on clinical need and not on the ability to pay.
According to research conducted by Baker et al. (2019) on the language of patient feedback, they found that
among the concerns that were raised as ‘urgent’ included not having access to services such as being referred to specialists; problems with booking medical appointments; lack of parking facilities especially disabled parking spaces; and parking being too expensive in general [30]. Such concerns raise issues related to the way hospitals are financed and the way the budget is managed. Whereas the NHS, is funded mainly from taxation and National Insurance contributions (NICs), bimaristans were mainly financed by Waqf (pl. Awqaf), which is a property that is dedicated to a beneficial cause in the hope to seek spiritual reward. The proceeds were
typically used to finance educational institutions, graveyards, mosques, shelters, and retirement homes
[31][32].
Waqf, however, was largely used to fund hospitals and medicines. The 50 hospitals in Cordoba were all financed
by waqf. In Istanbul, the waqf fund was used to establish a hospital for children [33]. Moreover, the waqf funds
were used not only to establish whole institutions but were also used to make improvements or provide specific
services. The waqf fund was used also to maintain and pay for the running costs of the bimaristans. For instance, funds would be used to offer clothing to patients as well as to provide plenty of healthy food. The patients’ eating habits were considered for prognosis. Surviving recipes from early Islamic cookbooks and bimaristan records reveal that meats, vegetables, and fruits were more common than common staples such as bread.
Interestingly, the discharge of patients seems to have been based on their their ability to consume a whole
chicken; viewed as a sign of well-being to be able to eat an equivalent of a three-course meal [34].
A recent example of a waqf-based clinic in a non-Muslim country is the MyintMyatPhu Zin clinic founded in 2009,
located in the middle of Mandalay, the cultural and Church religious centre of Buddhism in Burma. The land was
donated by two founders and additional contributors supported the building of the clinic. The clinic was established to show how Islamic teachings could play a significant role in the well-being of the people of
Myanmar irrespective of their beliefs [35].
3. Bimaristans and Europe
Bimaristans influenced the mindset of physicians in the Middle Ages. This section explores how the medicine
previously practised in Christian Europe was developed; the way Europe embraced the medical achievements of bimaristans; and importantly, how the bimaristans served as models of a patient-centred health care system.
3.1 Change of medical mindset
A major shift in the way medicine was approached was that the physicians focused more on health rather than
disease. Avicenna (from the Arabic IbnSina, d. 1037), in the Canon of Medicine, writes,
To medicine pertains the (study of the) human body — how its health is maintained; how it loses health.
To know fully about each of these we must ascertain the causes of both health and sickness. Now as
health and sickness and their causes are sometimes evident to the senses and sometimes only perceived monotheistic views attracted the Church which adopted by means of the evidence afforded by the various
symptoms, we must in medicine gain knowledge of the symptoms of health and sickness [36].
Diseases were not viewed by Muslim physicians as a divine punishment but as a result of the interaction of the
human body with its surroundings. Moreover, this led to finding the elementary cause of diseases and finding the treatment. An idea which Prophet Muhammad himself emphasised, ‘Allah did not create an illness except he also created for it a treatment. Those with knowledge are aware; whilst those who are ignorant, remain ignorant’ [37].This statement is likely the cause of Muslim scientists wanting to witness the truthfulness of to Muhammad’s statement and choosing to no longer remain ignorant of such life-changing knowledge. In this way, the bimaristans were not just places where patients were treated but where the spirituality of physicians and patients was strengthened as they witnessed diseases – that were once thought impossible to cure – being cured
before their eyes [38].
3.2 Development of the medicinal practice of the Church
The focus on saving the body as well as the soul was in a sense, unique to bimaristans. During medieval times, the Church made efforts to curb the spread of diseases and to tend to the care of the sick. The aim of the Church appears to have been the salvation of the soul since effective treatments had not developed [39]. Nevertheless, followers of the Abrahamic faiths were spiritually motivated to attend to the ‘physical needs’[40] of the sick often by female nurses, who kept patients warm and well fed, hence, the word ‘nurse’, which comes from the Latin nutricius or nutritius meaning nourishing [41].
The Church helped in establishing hospitals annexed to monasteries to tend to the care of the ill. The medicine of the time was based on Hippocrates’ theory of the four humors. Humorism is the idea that if the four liquids in the human body (phlegm, blood, yellow bile, and black bile) were out of balance then one would become sick. Galen developed humorism through the theory of opposites, by this he believed that bodily liquids could regain balance for instance by having a hot bath during cold weather to control excessive phlegm. This theory also gave rise to purging, bloodletting, and amputation of limbs [42]. However incorrect Galen’s theory, he concluded that the design of such a marvellous body meant that there must be a God who designed it. Galen’s monotheistic views attracted the Church which adopted his work. However, without the Church challenging Galen’s theories, it faced a great medical challenge during the great plague.
With the fall of the Roman Empire, the blueprints explaining the methods to repair aqueducts, toilets, and public baths too were lost. Access to clean drinking water declined and biological waste in public places increased. The foul smell and bad air gave rise to miasma theory which held that plagues were caused by rotting organic matter [43]. The Church also held the belief that plagues, as described in the Bible, were divine punishments for sins. Between 1000 and 1500 CE, over 700 hospitals next monasteries were set up in England by the Church [44]. Another belief during the time, which was rooted neither in Christianity nor Islam, was that the plague was due to the position of the planets. The Church encouraged regular prayer to God and to burn incense. Additionally, some Christians viewed making pilgrimage to holy sites as a way of atonement. Bearing in mind the theological and supernatural explanations, the plague is known to have travelled through the European trade routes through rats and fleas. Despite the many well-intended efforts of the Church, the physical cause of the plague appears to have remained unknown. On the other hand, the Muslim lands were also unable to curb the spread of the plague and casualties were high even in Cairo despite the QalawunBimaristan. However, physicians in bimaristans endeavoured to understand the cause of the plague based on empirical evidence.
3.3 Influence of bimaristans throughout Europe
The influence of bimaristans is still acknowledged in places across Europe today. In the scholars pavilion at Muslims, the UN office in Vienna are situated statues of Muslim physicians Rhazes (from the Arabic Muhammad ibn Zakariyya al-Razi, d. 925) and Avicenna. Chaucer (d. 1400), who is considered to be the founder of English poetic tradition as well as the greatest English poet of the Middle Ages, also included Rhazes and Avicenna among the greatest physicians ever known alongside Aesclepius (c.1250 BC) and Hippocrates [45].
Among the reasons why Europeans in the Middle Ages cherished the Muslim legacy was perhaps because much of European history would have been lost forever had the bimaristans not preserved European medicine. In 814 CEafter the death of Charlemagne, Latin European culture began to fade. However, this culture survived in Toledo, Spain [46]. Archbishop Raymond de Sauvetât (d. 1152) of Toledo established a translation institute where Arabic manuscripts, which were received from various locations, were translated into Latin. These Latin translations were then shared throughout Europe especially in France and Germany in the 17th century. Seeking medical knowledge from books, however, was still secondary. were the primary locations where medical knowledge was acquired first-hand.,
Bimaristans offered an opportunity for physicians, and the medical students, men and women, to pool their resources together becoming a place of medical training. Cordoba alone consisted of 50 major hospitals that treated physical and mental illnesses [47]. This new phenomenon gave rise to medical institutions emerging in Western Europe such as in Salerno, Padua, and Bologna in Italy, and Montpellier and Paris in France [46]. The harmonious relations between the Islamic East, Andalusia, and the Latin West in the 12th to the 14th century gave rise to European medical institutions that were comparable to bimaristans, such as the Hospital of Our Lady Mary of the Innocents in Valencia [48].
3.4 Patient-centred health care system
Bimaristans considered the needs of the patients and their families. In broad terms, these needs included spiritual, mental, physical, and social needs [49]. As the patients were most likely to have a religious affiliation, bimaristans included separate prayer rooms for the patients. For instance, the Bimaristan Al-Mansuriin Cairo contained prayer areas for Muslims and other followers of the Abrahamic faiths [50]. Areas of worship were included not only in hospitals but medical treatment was also made available to travellers on their way to Makkah. Understanding the importance of the annual Hajj for road bimaristans were also set up by philanthropists [51].
The bimaristans also considered the social needs of the patients. Muslim communities tend to value gender- specific services. Furthermore, bimaristans were needed in villages and rural areas as much as they were needed in cities. The Qur’an also encourages showing kindness to prisoners and so free medical care was also made available to prisoners [52].
The wards in bimaristans were separated by diseases as well as gender [53]. The Bimaristan Al-Mansurihad many , specialised wards. The hospital itself had two sections: one for men and the other for women. This aspect is important in Islamic culture as Muslim women tend to avoid exposing their bodies unnecessarily, especially to men outside of their families. However, since medical examinations may require exposing the abdomen or genitalia, men and women were provided with separate wards and where possible, women were treated by women. Catering for such needs inspired women to take Bimaristans up a career in medicine.
Considering the wider communities; those in the villages and peripheries Isa ibn Ali Al-Jarrah (d. 946) wrote to Abbasid Caliph Al-Muqtadirbillah [54]:
I thought of people who live in the peripheries and that among them are patients who do not receive any medical care because there are no doctors there. So, assign – May God prolong your life – some physicians to visit the peripheries; also a pharmacy containing drugs and syrups. They have to travel all through the peripheries and stay in each region enough time to perform treatment of patients, then they move to another one.
Likewise, Isa wrote regarding prisons:
I thought – May God prolong your life – of the imprisoned and they are exposed, due to their big number and their hard situation, to diseases; they are incapable to deal with their excretions or to meet doctors to seek their advice about diseases. You have – May God grant you honor – to assign physicians to visit them daily and they should carry with them drugs and syrups and all they need to treat the patients and cure illnesses with God’s will.This call was answered by Al-Muqtadir and a bimaristan for prisoners was built in circa 919, which was financed with 200 dinars monthly [54].
The bimaristans also made efforts to minimise patients’ anxiety and worries. Bimaristans were constructed on sites with fresh air and which were aesthetically pleasing. For instance, when Rhazes searched for a place in Baghdad to establish a bimaristan, he chose a place where pieces of meat would take the longest to rot [55]. Bimaristans also appear to have promoted the restoration of health where patients felt that they were not left to die. Instead, bimaristans were built within the cities where they could be visited by families and friends and hope to rejoin society upon recovery. Bimaristan Al-Adudiwas built by the River Tigris. The water from the river would flow into the courtyard of the bimaristan and through the halls before it reconnected to the Tigris [56][57].
Perhaps, the greatest worry for patients is not understanding the information they are given. Prophet Muhammad taught to speak to people in a manner that was comprehensible for the audience and to avoid esoteric language. He was known to be succinct and repetitive in his main points and the hadith literature contains a plethora of similes, examples, analogies, as well as questioning the audience to assess their understanding. Low health literacy is likely among the elderly and ethnic and racial minorities [58]. When Salman, the renowned elderly Persian immigrant companion of Muhammad, fell ill on one occasion, Muhammad checked on his well-being in Farsi [59]. An interesting parallel to note is how Muhammad himself welcoming foreign words led to hospitals in Arab lands to be known as bimaristans; derived from bimar – a sick person, and -stan – place, meaning ‘a place where patients reside’ [60]. The very use of this Persian word in Arab lands reveals a process of international social healing and leaving behind old enmity. In medical practice, the physicians in the bimaristans would be expected to speak to patients in a way that was accessible to the patients to increase adherence.
Furthermore, as soon as patients were admitted to the bimaristans, their clothes and possessions would be kept safely in a place of trust by the security team [61]. Patients were also separated into different wards according to an initial diagnosis. Three separate halls would be found which were allocated to patients with a) internal diseases, b) patients with trauma and fractures, and c) communicable diseases. Because contagious diseases are highly likely to create fear and panic among patients, they would not be kept in the same halls. Likewise, patients with severe mental illnesses exhibiting aggression were also isolated safely and securely [62].
Along with bimaristans being known as places for the sick to seek medical treatment, they were also appealing for trainees to learn medical knowledge and specialise in different fields of medicine and surgery. The medical education system was based on an Islamic ethos of valuing everyone involved in the bimaristans, from respecting the senior staff to helping develop the junior staff and creating an overall supportive work environment. The participation of children in bimaristans is also noteworthy. Children would volunteer to help with administrative tasks [63].
Such practises reveal clear cultural differences between now and the Middle Ages regarding child labour. Nevertheless, inspiring future generations to value health care can be promoted in creative ways. During the COVID-19 pandemic, a group of enthusiastic children from different ethnicities created videos in Bengali, Gujarati, Punjabi, and Urdu among other South Asian languages to encourage the elderly in their communities to take the vaccine [64].
4.Bimaristans as educational institutes
The educational aspect of the bimaristans focused on the importance of a positive rapport in the doctor-patient relationship. Faith and spirituality also appear to have played a major role in motivating health care providers to build resilience to their career challenges and avoid burnout.
4.1 Mentor-trainee relationship
The education system involved senior staff being role models for trainees and junior staff. From the onset,  despite the hierarchy of the staff and management structure, the Qur’an states, that ‘above anyone who possesses knowledge, there is one with greater knowledge’ [65]. This verse helps to reduce hubris and instil a realisation within the workforce that every and individual has something unique to offer. Prophet Muhammad himself once said to a physician, ‘Allah is the one who cures, you are the one who is gentle’ [66]. and drugs were readily available [73]. The etymology ofThis hadith promotes a patient-centred attitude whereby the role of the physician is to be gentle with the patient who is experiencing a difficult time, whether that be through for instance CPR or heart surgery. also promotes the idea that the medical staff are a means through which healing occurs. This idea is internalised and expressed by Muslims in the expression ‘Qaddarallah’ meaning ‘As Allah expected’; a phrase Prophet Muhammad was that would have also resonated with Christian physicians through Christ’s parable of the Master and servant [67].
despite the hierarchy of the staff and management structure, the Qur’an states, that ‘above anyone who possesses knowledge, there is one with greater knowledge’ [65]. This verse helps to reduce hubris and instil a realisation within the workforce that every and individual has something unique to offer. Prophet Muhammad himself once said to a physician, ‘Allah is the one who cures, you are the one who is gentle’ [66]. and drugs were readily available [73]. The etymology ofThis hadith promotes a patient-centred attitude whereby the role of the physician is to be gentle with the patient who is experiencing a difficult time, whether that be through for instance CPR or heart surgery. also promotes the idea that the medical staff are a means through which healing occurs. This idea is internalised and expressed by Muslims in the expression ‘Qaddarallah’ meaning ‘As Allah expected’; a phrase Prophet Muhammad was that would have also resonated with Christian physicians through Christ’s parable of the Master and servant [67].
To be a part of the healing process in bimaristans, however, required training and showing competence. Notably, bimaristans promoted the assurance that physicians needed to be accredited and licensed by senior physicians to practise medicine [68]. Arguably, in 1207, the Qarawiyyin University in Fez honoured Dr Abdellah Ben Saleh El-Koutami as the first physician to have been awarded Doctor of Medicine. The document, which survives until today, highlights that physicians were expected to be spiritual as well as have excellent relational skills [69]. This approach is what likely gave rise to an unprecedented high quality of medical practice. Physicians also specialised in different diseases. The specialities gave rise to the separation of patients in different wards depending on the nature of the diseases.
Clear expectations were made known to trainees. When Adud Al-Dawlah (d. 983) established the bimaristan in western Baghdad, he made known that out of a hundred physicians, only 24 would be selected for work [54.] Physicians were also reminded that they would be held accountable in the case of any death. Physicians were, therefore, expected to keep a record of all the medication they prescribed until the patient was either cured or died [70]. If a patient died, then the chief physician would review the prescriptions to evaluate the treatment and conclude whether the death was natural or due to negligence. In the case of negligence, the physician was held accountable and was liable to pay blood money to the family of the deceased. The records themselves would be archived for future research. Training the staff to perform their duties competently was, therefore, of great importance at the bimaristans [71].
‘Make matters easy, do not make them difficult’, instructed Prophet Muhammad [72]. Bimaristans made efforts to make easier the lives of staff and patients. Staff members were provided with all the medical instruments and apparatuses that were necessary for the time. Pharmacies, known as Khizanat al-sharab or Saydaliyah were annexed to bimarsitans so that medication, syrups, and drugs were readily available [73]. The etymology of the English noun ‘syrup’ is of Arabic origin from the word sharab meaning beverages [74]. The word was adopted as a result of the widespread medicinal syrups that were made available throughout European dispensaries based on recipes prepared by chemists for the bimaristans [46].
Prophet Muhammad was a strong advocate of documentation as is evident from the Qur’an, which encourages documenting financial transactions [75]. Muhammad allowed prisoners of war to free themselves by teaching literacy skills [76]. Muhammad himself would often use his staff to draw diagrams in the sand to visually explain abstract concepts. This combination of writing and illustrations was also encouraged among Muslim physicians which led to grand medical libraries. For instance, Egypt’s Ibn TulunBimaristan is known to have had a collection of over 100,000 books on medicine [77].
Leading physicians supported fellow physicians in the medical field by authoring instruction manuals. For instance, Albucasis (from the Arabic Abul Qasim Al- Zahrawi, d. 1013) wrote his 30-volume medical encyclopediaKitab al-Tasrif li-man ‘Ajizja ‘an al- Ta’lif(meaning ‘The arrangement of medical knowledge for one who is unable to compile a manual for himself’)[78], in which he wrote sections on medicine, orthopaedics, ophthalmology, pharmacology, and nutrition[79] and discussed over 300 diseases and their treatments [80]. The last volume also describes surgical procedures and instructions on how to use more than 200 surgical instruments. Albucasis described ways to treat congenital hand deformities such as polydactyly and syndactyly as well as ways to treat hypospadias and genital reconstruction. Other procedures which Albucasis covered include oculoplastics, eyelid surgery, gynecomastia, and breast surgery [81]. The work was first translated into Latin in 1519 under the title Liber theoricaenecnonpracticaeAlsaharaviiand served as a reference guide in Europe until the 18th century.The most eminent surgeon of the European Middle Ages Guy de Chauliac in his work Chirugia magna (meaning ‘Great Surgery’, completed in 1363), quoted al-Tasrif over 200 times [82]. An instruction to ‘Seek knowledge even unto China’[83] is also attributed to Prophet Muhammad. Such instruction may have alluded to learning Chinese medicine. Excelling in response to this instruction, Muslim physicians reached a reputation to the point that the Chinese came to learn medicine from Rhazes [84].
4.2 Appreciating the diversity of staff
The practice of medicine is a joint global contribution of many civilisations and is inextricably intertwined and one which requires diverse representation [85]. The senior medical team in bimaristans would consist of diverse members. Prophet Muhammad valued and promoted diversity and appreciated the invaluable experience of those around him irrespective of gender, religion, and race. Muhammad’s caller to prayer was Bilal, an Ethiopian who was once a slave in Makkah; Muhammad acted on the advice of Salman when the latter advised digging a trench around the city; a Persian military tactic. At the treaty of Hudebiya, Muhammad was the first to terminate his pilgrimage after being advised by his wife Umm Salama. At a time when the status quo was for free Arab men to make important decisions, Muhammad demonstrated the value of allowing a voice to all people. Such opportunities inspired women to lead in medicine [86]. Bint Shihab al-Deen, in 1627 became the masheekhat al-tibb, meaning the chief physician at the Bimaristan Al-Mansuri. Such an ecumenical approach inspired bimaristans to also create opportunities to collaborate for leading physicians irrespective of religion, gender, and race [87]. Bimaristans became the discussion place for physicians who were interested in challenging Galenic medicine; they were welcomed by Muslim physicians who were interested in looking at medicine through the lens of Islamic medical ethics.
With Muhammad’s descendants marrying into cultures, this would have made working with Arab Muslims easier for people of other faiths, as well as non- Arabs. Al-Mansur established the Bait al-Hikma, meaning the house of wisdom. This institute became library of academic work. Great scholars of Syrian, Hebrew, and Persian heritage belonging to several faith groups including Islam, Christianity, Judaism, and Zoroastrianism, gathered to translate Greek, Latin, even Sanskrit works into Arabic.
The collaborative environment of bimaristans also promoted the idea that even senior physicians had much to learn from other scholars. This attitude would then be instilled within the trainees, who would also realise that mistakes are inevitable, however, the more effective the collaboration, the better the outcome would be moving forward. The physicians worked in shifts to ensure that senior physicians were available to support the trainee staff morning and night [88]. Trainees would gather around the senior physicians to learn how to examine patients as well as learn the way to appropriately interact with patients. Aside from teaching trainees practically, medical theory was also taught through lectures. Theoretical medical knowledge was taught through lecture rooms and libraries as was found in the bimaristans at Baghdad, Damascus, and Cairo in the 10th century [89].
The trainees in these bimaristans would enter the field knowing that medicine would be a challenging career yet one that would be spiritually fulfilling. The senior staff would foster the resilience that trainees needed through positive and active behaviours; that is by demonstrating hard work, constant reflection, and discussions on ways to improve by challenging and pushing the boundaries of medicine.
The spiritual and religious aspects of bimaristans are likely to have played a large role in inspiring and motivating trainees to build the resilience required for a career in medicine. Leading physicians also held prominent religious status; Averroes (from the Arabic Ibn Rushd, d. 1198) was a leading jurist of the Maliki school of Islamic jurisprudence and also held the position of chief judge in Cordoba. Ibn al-Nafis (d. 1288), a pioneer physician in the history of Islamic medicine who worked at Bimaristan Nur al-Din (see images 5 and 6 below) in Damascus also worked later in Cairo as a leading Shaf’I jurist [90]. Part of the Muslim culture of the bimaristans was the prohibition of drinking alcohol, gambling, any other addictive behaviour for entertainment or celebratory purposes, or to relieve stress. Excessive alcohol intake, drug misuse, and relationship breakdown are all associated with burnout, which could adversely affect patient care [91]. The Islamic alternatives would be to enjoy non-alcoholic feasts, gifting, and establishing a culture of praise and gratitude. Trainees would view success as a blessing and view failure as understanding that they were still on a journey.
4.3 Cultivating a trusting doctor-patient
Islamic medical ethics also focuses on trust between the doctor and patient. Ishaq ibn Ali Ruhawi (d.931) wrote extensively on the doctor-patient relationship in his most celebrated work Adab al-Tabib (Practical Ethics of the Physician)[94]. Trust could be built on a physician’s experience or knowledge about a specialised area of medicine.
 Figure 5. Bimaristan Nur al-Din from the inside(Damascus, Syria)[92]
Figure 5. Bimaristan Nur al-Din from the inside(Damascus, Syria)[92]
Figure 6. Bimarist an Nur al-Din from outside (Damascus, Syria)[93]
However, there are additional factors that could be at play, which may affect the doctor-patient relationship. Many fatwas related to medicine often focus on the doctors themselves as the subject of the fatwas [95]. Considering the socio-cultural interests of Muslim patients, a patient’s level of anxiety and distress may be caused as a result of a negative experience [96]. For many Muslim patients, the doctor’s gender, the language of communication, personality, and moral conduct all play a role in the decision-making process when seeking medical treatment. A negative experience or an experience that does not meet the expectations of the patient may affect a patient’s decision to take any prescribed medication and may also result in the patient not returning for a second visit [97].
From an Islamic perspective then, the first encounter between a patient and the doctor requires meeting certain expectations that include a range of aspects including the characteristics of the doctor as well as meeting socio-cultural requirements. Importantly, this aspect of medical ethics should be valued especially because the first interaction has intrinsic value as well as it could have an impact on relevant clinical outcomes [98].
A greater focus on diversity and welcoming different perspectives in the NHS could help pool together a wide range of experiences. Bimaristans were places that attracted patients and physicians from different places due to their ecumenical approach to inviting a diverse team to advance in the field of medicine. The attitude of the workforce in bimaristans influenced European medicine whereby comparable institutes began to emerge across Europe. Physicians and trainees in bimaristans were supported in an environment that focussed on the patients’ well-being whilst highlighting that physicians play a vital part in the medical process. The motivation to be a resilient member of this process was nurtured through the spiritual ethos of the bimaristans.
Although religion at the workplace remains a private matter, perhaps religion and spirituality are reaching a stage where its mention creates unease or even discrimination. A physician’s faith and belief are likely to play a role in building a strong work ethic [99]. Moreover, referring to such a great period of history as the ‘dark ages’ is ironic if health care providers are kept in the dark about the great medical, surgical, and pharmaceutical advancements that were taking place [100][101]. Positive and constructive discussions on faith and medical history may prove to be healthy to understand better what motivates health care providers. On the other hand, institutional racism and a legacy of mistreatment of patients have led to a lack of trust in the NHS as has been shown in the reluctance of ethnic minority groups to register as organ donors as well as in their low uptake of vaccines [102]. In medical textbooks, a representation of influential male and female physicians from the Middle Ages from various cultures and places could prove to be more inviting to medical students.
Bimaristans appear to have provided the workforce with the essential equipment and tools needed to complete jobs effectively – either through government funding or through the awqaf system. Such funding sources could be used in our time to set up courses on building interpersonal and soft skills. Additionally, health care staff could be taught cultural competence to better support patients. Translation services could also be developed with such funds. Moreover, the idea of funding evening clinics may help address the concerns of Muslim patients in Ramadan when they are likely to avoid medication and appointments during daylight hours due to devoting time to religious matters whilst fasting[103].
Importantly, the workforce at bimaristans was the driving force behind medical advancements. The workforce was a product of the modest and resilient culture that was promoted within the bimaristans. Hospitals today provide cutting-edge treatments using advanced technological tools that were unimaginable in the Middle Ages. However, we need to remind ourselves that patients expect to build rapport with trustworthy human physicians before agreeing to the use of any sophisticated technology.
The NHS in many ways mirrors the once-great bimaristans. The NHS continues to attract physicians from around the world. In 1971, 31% of all doctors in England were born and qualified abroad. By 2016, over 9,200 of the 29,200 Muslim staff held specialised positions. Of the 61,900 doctors who were asked about their religion, 15% disclosed that they were Muslims. Interestingly, 15% is an over-representation since the Muslims make up only 5% of the national populace [104]. Muslim health care providers in the UK today do not work separately in bimaristans but rather make up the very fabric of the NHS. British Muslim organisations like the British Islamic Medical Association (BIMA), the Muslim Doctors Association (MDA), AlBalagh Academy, and Muslim Doctors Cymru (MDC) continue to promote Islamic medical ethics, offer a platform for physicians to engage in academic research, and help junior doctors develop personally and professionally. Furthermore, during the COVID-19 pandemic, a number of British Muslim communities offered their local mosques as vaccination centres [103].
Further collaboration between the NHS, Public Health, and current Islamic medical organisations could help to refine medical ethics, raise standards of health care, deliver a better patient-centred health care system, and create an inclusive educational culture wherein senior staff and trainees of all backgrounds can take pride in their careers. Moreover, greater inclusion efforts are likely to attract philanthropists. In closing, for health care providers to attain cultural proficiency – valuing pluralism, respect, and openness to diverse ways of viewing health care are strongly advise
References
1. Moberly, T. Providing care based on need and free at point of delivery is NHS’s greatest achievement, say BMJ readers. BMJ, 2018, 361.
2. 2. Al-Bukhari, M. I. Sahih al-Bukhari; Kitabtafsir al- Qur’an; Bab fasanuyassiruhuli’l ‘usra. Beirut,Lebanon: Dar Tauq al-Naja; 2001.
3. Al-Bukhari, M. I. Sahih al-Bukhari; Kitab al-qadar; Bab fi’lqadar. Beirut, Lebanon: Dar Tauq al-Naja;2001.
4. The Holy Qur’an: chapter 5, verse 32. This verse from Sura al-Ma’idah appears to refer to the Mishnah Sanhedrin 4:9; Yerushalmi Talmud, Tractate Sanhedrin 37a, which reads: “… whoever saves a life, it is considered as if he saved an entire world”.
5. Ebrahim, A.F.M. and Padela, A. The Islamic juridical principle of dire necessity (al-darura) and its application to the field of biomedical interventions In: Aasim P. (ed.). Medicine and Shariah: A Dialogue in Islamic Bioethics. Notre Dame, Indiana: University of Notre Dame Press; 2021. p. 57-70.
6. Ibn Abi Shaibah, A. Musannaf; Kitab al-zuhd; ma dhukira an nabiyyinafi’zzuhd. Riyadh, Saudi Arabia: Dar al-Fikr al-Mu’asir; 1988.
7. Al-Ghazal, S.K. The influence of Islamic Philosophy and Ethics on the Development of Medicine during the Islamic Renaissance. JISHIM, 2004, 3(6), 3-7.
8. Amr, S.S. and Tbakhi, A. Jabir ibn Hayyan.Annals of Saudimedicine. 2007, 27(1), 52-3.
9. Kraus, P. Jabir ibn Hayyan: [Dschabir] Contribution à l’histoire des idées scientifiques dans l’Islam (Vol II. Jâbir et la science grecque). Cairo, Egypt: Imprimerie de l’Institut Français d’Archéologie Orientale; 1943.
10. Al-Tabarsi, R.D. Makarim al-akhlaq; Al-bab
fasl 1: fi adaab al-maridhwa’la’idwailajih; fi thawab al-mareedh. Beirut, Lebanon:Mu’assasat al-Tarikh al-‘Arabi; 2004.
11. Madelung, W. Encyclopædia Iranica;ALĪ AL-REŻĀ
[Internet]; 2012 Dec 30 [cited 2021 Jun 2].
Availablefrom: https://iranicaonline.org/articles/ali-
al-reza
12. Ibn Abi Shaibah, A. Musannaf;Kitab al-tibb; Man
raxasa fi al-dawawattibb. Riyadh, SaudiArabia: Dar
al-Fikr al-Mu’asir; 1988.
https://dailynewsegypt.com/2019/12/07/bimaristan-
al-muayyad-one-of-the-worlds-largest-hospital-is-
locked-behind-islamic-cairos-gates/
13. Al-Sijistani, A.D. Sunan Abi Dawud;Kitab al-diyaat;
Bab fi man tatabbabbighairilmf’a’nat. Beirut,
Lebanon: Dar Ehia al-Tourath al-Arabi; 2000.
14. Dols, M.W. The Leper in Medieval Islamic Society.
Speculum. 1983, 58, 891-916.
https://twitter.com/IslamScienceNet/status/10811251
78661371904/photo/1
15. Dols, M.W. Insanity and its treatment in Islamic
Society. Medical History, 1987, 31, 1-14.
16. Abou-Saleh, M.T. and Salloum, I.M. Bimaristan
Arghun Al-Kamili in Aleppo, Syria: A mental
hospital with unique architecture designed to meet
patient need in medieval Islam (1354 AD). Arab
Journal of Psychiatry. 2020, Nov 1, 31(2), 191-195.
https://www.wikiwand.com/en/Qalawun_complex
17. Gagnon, B. BimaristanArghun Al-Kamili [Image];
N.D [cited 2021 Aug 7]. Available from:
https://archiqoo.com/locations/bimaristan_arghuni.php
18. Smith, V. Clean: A History of Personal Hygiene and
Purity. Oxford, UK: Oxford University Press; 2008.
19. Sabri, A. Al-ri’aya al-sihhiyyafi’l Islam (Health care
in Islam) [Internet]; 2015 Aug 28 [cited 2021 Jun 2].
Available from:
https://www.alkhaleej.ae/-في-ةيالصح-ةياالرع/حقمل
اﻹسﻼم
20. Ragab, A. The Medieval Islamic Hospital.
Cambridge, UK: Cambridge University Press; 2015.
21. Jan, R. Rufaida Al‐Asalmiya: the first Muslim nurse.
Image: The Journal of Nursing Scholarship. 1996,
28(3), 267-8.
22. Dols, M.W. The Origins of the Islamic Hospital:
Myth and Reality. Bull. Hist. Me, 1987, 61, 367-390.
23. U.S. National Library of Medicine. Islamic culture
and the medical arts: Hospitals [Internet]; 1994 April
15 [cited 2021 Jun 2]. Available from:
https://www.nlm.nih.gov/exhibition/islamic_medical/
islamic_12.html
24. Daily News Egypt. Bimaristan Al Muayyad, one of
the world’s largest hospital, is locked behind Islamic
Cairo’s gates [Image]; 2019, Dec 7 [cited 2021 Aug
7]. Available from:
25. Islam & Science. Hospital Development In Muslim
Civilisation [Image]; 2019, Jan 4 [cited 2021 Aug 7].
Available from:
26. Wikiwand. Qalawun complex [Image]; N.D [cited
2021 Aug 7]. Available from:
27. Saad, B. and Said, O. Greco-Arab and Islamic herbal
medicine: traditional system, ethics, safety, efficacy,
and regulatory issues. Hoboken, New Jersey: John
Wiley & Sons, 2011.
28. Clark, D. Population of Northern Ireland from 1971
to 2020 [Internet]; 2021 Jun 29 [cited 2021 Jun 29].
Available from:
https://www.statista.com/statistics/383733/northern-
ireland-population-timeline-uk/
29. Tschanz, D.W. Bimaristans and the rise of modern
health care systems Aspetar Sports Med J. 2017,
6(2), 438-443.
30. Baker, P., Brookes, G. and Evans, C. The language
of patient feedback: A corpus linguistic study of
online health communication. New York, NY:
Routledge; 2019.
31. Vishwanath, A. Explained: How a waqf is created,
and the laws that govern such properties [Internet];
2019 Oct 17 [cited 2021 Jun 3]. Available from:
https://indianexpress.com/article/explained/explained
-how-a-waqf-is-created-and-the-laws-that-govern-
such-properties-6072476/
32. Al-Hassani, S. Hospital development in Muslim
civilisation [Internet]; 2020 Oct 26 [cited 2021 Jun
3]. Available from:
https://www.historytoday.com/archive/feature/medie
val-hospitals-england
33. Al-Syed, A.M. Al-Waqf al-Islamiwa al-dawr al-
ladhila’ibahu fi al-Numuw al-Ijtima’i fi al-Islam
[Islamic Waqf and the role it played in social
development in Islam]. Islamabad, Pakistan:
International Islamic University Islamabad, 1983.
34. Reinarz, J. Towards a history of hospital food. Food
and History. 2016. Jan, 14(1), 1-2.
35. Htay, S.N., Salman, S.A., Myint, S. and Ilyas, H.
Integrating zakat, waqf and sadaqah: MyintMyatPhu
Zin clinic model in Myanmar. Tazkia Islamic
Finance and Business Review. 2014, Mar 9, 8(2),
170-186.
36. Avicenna. The Canon of Medicines (Tr. Oskar
Cameron Gruner). New York, NY: AMS Press;
1973.
37. Ibn Abi Shaibah, A. Musannaf; Kitab al-tibb;
Manraxasa fi al-dawa wat tibb. Riyadh, Saudi
Arabia: Dar al-Fikr al-Mu’asir; 1988.
38. Abdel-Halim, R. 1001 Cures: Introduction to the
History of Islamic Medicine; Human Anatomy and
Physiology in the Medieval Islamic Era. Kindle
edition; 2021.
39. Tschanz, D. W. The Islamic roots of the modern
hospital [Internet]; 2017 Apr [cited 2021 Jun 3].
Available from: https://www.aramcoworld.com/Articles/March-
2017/The-Islamic-Roots-of-the-Moddern-Hospital
40. The Epistle of James, 2:16.
41. Whaley, L. The healing care of nurses. In: Leigh W.
(ed.). Women and the Practice of Medical Care in
Early Modern Europe, 1400—1800. London, UK:
Palgrave Macmillan; 2011. p. 112-130.
42. Stapelberg, M-M. Through the darkness: Glimpses
into the history of western medicine. London, UK:
Crux Publishing; 2016.
43. Last, J.M. ‘miasma theory’. A dictionary of public
health. Oxford University Press, 2007.
44. Dainton, C. Medieval Hospitals of England. History
Today, 1976, 26(8). Available from:
45. Skeat, W. W. The complete works of Geoffrey
Chaucer edited, from numerous manuscripts. Oxford,
UK: Clarendon Press; 2007.
46. Farag, F.R. Why Europe Responded to the Muslims’
Medical Achievements in the Middle Ages. Arabica.
1978. Sep 1, 25(Fasc. 3), 292-309.
47. Thorne, K. Diversity and Coexistence: Towards a
Convivencia for 21st Century Public Administration.
Public Administration Quarterly. 2013. 37(3), 491-
528.
48. Pérez, J., Baldessarini, R.J., Undurraga, J. and
Sánchez-Moreno, J. Origins of psychiatric
hospitalization in medieval Spain. Psychiatric
Quarterly. 2012. 83(4), 419-30.
49. Al-Ghazal, S.K. The Origin of Bimaristans
(Hospitals) in Islamic Medical History. Foundation
for Science, Technology and Civilisation, 2007
https://muslimheritage.com/uploads/The_Origin_of_
Bimaristans_in_Islamic_Medical_History.pdf
50. Islam Message. Islam and Sience 7 [Internet]; 2020
Nov 5 [cited 2021 Jun 4]. Available from:
https://islammessage.org/en/article/5681/ISLAM-
AND-SIENCE-7
51. Ibn Kathir, I.U. Al-Bidayawa’nnihaya. Damascus,
Syria: Dar al-Fikr; 1986.
52. The Holy Qur’an: chapter 76, verse 8.
53. Kump, W.L. Historic hospitals. Financing the
Maristan of Qalaun. Minnesota Medicine. 1974,
57(6), 464.
54. Al-Qifti, J. Ikhbar al-ulama bi akhbar al-hukama.
Beirut, Lebanon: Dar al-Kutubal’Ilmiyah; 2005.
55. Afshar, A., Steensma, D.P. and Kyle, R.A. Razi:
Critical Thinker, and Pioneer of Infectious Disease
and Ophthalmology. Mayo Clinic Proceedings. 2020,
95(5), e53-e54.
56. Miller, A.C. Jundi-Shapur, bimaristans, and the rise
of academic medical centres. Journal of the Royal
Society of Medicine. 2006, 99(12), 615-617.
57. Hamarneh, S. Development of Hospitals in Islam.
Journal of the History of Medicine and Allied
Sciences. 1962, 18(3). 366-384.
58. Trinh, N.H. and Bernard-Negron, R. Mental health
issues in racial and ethnic minority elderly. Current
psychiatry reports. 2019, 21(10), 1-6.
59. Al-Tabarsi, R.D. Makarim al-akhlaq. Al-bab 11; Al-
fasl 3; fi’listishfabis-sadaqa wad du’a was salah; salat
al-a’ma. Beirut, Lebanon: Mu’assasat al-Tarikh al-
‘Arabi; 2004.
60. Anand, J.K. Etymology of the word ‘Bimaristan’.
Journal of the Royal Society of Medicine, 2007,
100(2), 69.
61. Al-Maqrizi, A.A. Al-Mawa’izwa’lEtibaarbidhikr al-
khutatwa’lathaar. Cairo, Egypt: Maktabah al-
Thaqafah al-Diniyah; 2002.
62. Noshrawy, A.R. The Islamic Bimaristans in the
Middle Ages (Arabic Translation by M. Kh. Badra).
The Arab Legacy Bul, 2007, 21, 202.
63. Al-Sharrah, Y.A. The Arab tradition of medical
education and its relationship with the European
tradition. Prospects. 2003, 33(4), 413-25.
64. BBC News. Covid-19: Breaking down Asian vaccine
myths in Lancashire [Internet]; 2021 Jan 13 [cited
2021 Jun 4]. Available from:
https://www.bbc.co.uk/news/uk-england-lancashire-
55630726
65. The Holy Qur’an: chapter 12, verse 76.
66. Al-Sijistani, A.D. Sunan Abi Dawud; Kitab al-
tarajjul; Bab fi’lkhidaab. Beirut, Lebanon: Dar Ehia
al-Tourath al-Arabi; 2000.
67. Gospel of Luke: chapter17, verses 7-10.
68. Syed, I.B. Islamic Medicine: 1000 years ahead of its
times.Jishim, 2002, 2, 2-9.
69. Cherradi, Y. About the First Available and
Documented MD Certificate Delivered in the World:
“IJAZAH”. Historical Focus, 2020, 4(3), 679-683.
70. Rooney, A. The History of Medicine. New York,
NY: Rosen Publishing Group; 2013.
71. Ibn al-Ukhuwwa, D. Ma’alim al-qurbafīahkām al-
hisba. London, UK: Lukac; 1938.
72. Naisapuri, M. H. Sahih Muslim; Kitab al-jihad wa al-
siyar; Bab fi’lamrbi’ttaysirwatark al-tanfir. Beirut,
Lebanon: Dar Ihya al-Turath al-Arabi; N.D.
73. Atiyeh, M. Arab hospitals in history. Annals of Saudi
Medicine. 1982, 2(2): 121-126.
74. Oxford English Dictionary; ‘Syrup’ [Internet]; 1919
[cited 2021 Jun 4]. Available from:
https://www.oed.com/view/Entry/196652?result=1&r
skey=1uNKkF&
75. The Holy Qur’an: chapter 2, verse 282.
76. Ibn Qayyam, M. Zad al-ma’ad fi hadykhair al-ibad.
Beirut, Lebanon: Dar al-M’arifah; 2009.
77. Latif, A. Development of Pharmacology (Ilmul
Adwia) During Abbasid Period and its Relevance to
Modern Age. Hyderabad, India: Prowess Publishing;
2019.
78. Al-Zahrawi, K. Kitab al-Tasrif li-man ‘Ajizja ‘an al-
Ta’lif. Tehran, Iran: Institute of Islamic Studies;
1996.
79. World Digital Library. Theoretical and Practical
Book by Al-Zahrawi [Internet]; 2018 Apr 3 [cited
2021 Jun 4]. Available from: https://www.wdl.org/en/item/9552/
80. Al-Ghazal, S.K. The history of Islamic medicine – A
light in the dark ages. Qabasaat mudhi’a min tarikh
al-tibb al-Islami, Humus EVi [YouTube]; 2021, Jul
18 [cited 2021, Jul 18]. Available from:
81. Al-Ghazal, S.K. Al-Zahrawi (Albucasis) – A Father
of Operative Plastic Surgery in Europe. JBIMA,
2020, 5(2), 34-39.
82. Al Hassan, S.M. Abul-Qasim Al-Zahrawi: The Great
and Pioneer Muslim Surgeon and Inventor of many
Surgical Instruments. Peshawar Islamicus. 2017,
8(2), 45-60.
83. Ibn al-Jawzi, J. Al-mawdou’aat. Al-Madinah, KSA:
Al-makataba al-Salafiyya; 1966.
84. Al-Nadim, M. Al-Fihrist; Qalam al-Sine. Beirut,
Lebanon: Dar Al-Ma’rifa; 1978.
A Dialogue in Islamic Bioethics. Notre Dame,
Indiana: University of Notre Dame Press; 2021. p.
39-56.
85. Le, T., Bhushan, V. and Sochat, M. First Aid for the
USMLE Step 1 2021: A student-to-student guide.
New York, NY: McGraw-Hill Education; 2021.
86. Al-Ghazal, S.K. and Husain, M. Muslim Female
Physicians and Health care Providers in Islamic
History. JBIMA, 2021, 7(3), 23-30.
87. Al-Saeed, A. Al-Tibbwara’idatihulmuslimat. Al-
Zarqa, Jordan: Maktabat al-Manar; 1985.
88. Majali, A. and Sahar, A.M. Contribution of Medieval
Islam to the Modern Hospital System. Historical Res
Lett. 2017, 43, 23-28.
89. Islamic Hospitals Source. Qatar Medical Journal,
2011, 20(1), 1.
90. Al-Ghazal, S.K. Ibn Al-Nafis and the Discovery of
Pulmonary Circulation. Foundation for Science
Technology and Civilisation, April 2007.
https://muslimheritage.com/uploads/Ibn_al-
Nafis_and_Discovery_of_Pulmonary_Circulation1.p
df
91. Forsythe, R.O. and Suttie, S.A. Enhancing junior
doctors’ working lives. Surgery (Oxford). 2020,
38(10), 607-611.
92. Frank, H. Nur al-Din Bimaristan [Image]; N.D [cited
2021 Aug 7]. Available from:
https://archiqoo.com/locations/nuri_bimaristan_dama
scus.php
93. MIT Libraries. Bimaristan Nur al-Din [Image]; N.D
[cited 2021 Aug 7]. Available from:
https://dome.mit.edu/handle/1721.3/164760
94. Levey, M. Medical ethics of medieval Islam with
special reference to Al-Ruhawi’s ‘Practical Ethics of
the Physician.’ Transactions of the American
Philosophical Society, 1967, 57(3), 1-00.
95. Rispler-Chaim, V. The Relationship between
Religion and Medicine: Insights from the Fatwā
Literature. In: Aasim P. (ed.). Medicine and Shariah:
https://www.mend.org.uk/islamophobia-awareness-
month-muslim-contributions-to-the-nhs/
96. Dean, M. and Street, R.L. A 3-stage model of
patient-centered communication for addressing
cancer patients’ emotional distress. Patient
EducCouns. 2014, 94(2), 143-8.
97. Dang, B.N., Westbrook, R.A., Hartman, C.M. and
Giordano, T.P. Retaining HIV patients in care: the
role of initial patient care experiences. AIDS Behav.
2016, 20(10), 2477-87.
98. Dang, B.N., Westbrook, R.A., Njue, S.M and
Giordano, T.P. Building trust and rapport early in the
new doctor-patient relationship: a longitudinal
qualitative study. BMC Medical Education. 2017
Dec, 17(1), 1-0.
99. Al-Ghazal, S.K. Medical ethics in Islamic history at a
glance. JISHIM, 2004, 3, 12-3.
100. Al-Hassani, S.T.S. Thousand years of missing
history. Found SciTechnolCivilis, Oct 2003.
101. Al-Ghazal, S.K. and Tekko, I.A. The valuable
contributions of Al-Razi (Rhazes) in the history of
pharmacy during the Middle Ages. JISHIM, 2003,
2(9), 9-11.
102. Forster, A.S., Rockliffe, L., Chorley, A.J., Marlow,
L.A., Bedford, H., Smith, S.G. and Waller, J.
Ethnicity-specific factors influencing childhood
immunisation decisions among Black and Asian
Minority Ethnic groups in the UK: a systematic
review of qualitative research. J Epidemiol
Community Health. 2017, 71(6), 544-9.
103. Maravia, U. COVID-19 Intra-muscular vaccinations
during Ramadan: Vaccines whilst fasting. JBIMA,
7(3), 3-11.
104. MEND. Islamophobia Awareness Month: Muslim
Contributions to the NHS [Internet]; 2019 Nov 6
[cited 2021 Jun 5]. Available from: